REVIEW ARTICLE | https://doi.org/10.5005/jp-journals-10082-02257 |
Radiological Findings in COVID-19 Pneumonia
1–3Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India
4Department of Radiodiagnosis, Valduce Hospital, Como, Italy
Corresponding Author: Padhmini Balasubramaniam, Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India, Phone: +91 9487139946, e-mail: drbpadhmini@gmail.com
How to cite this article Balasubramaniam P, Varma LS, Das N, Lomoro P. Radiological Findings in COVID-19 Pneumonia. J Basic Clin Appl Health Sci 2020;3(2):59–64.
Source of support: Nil
Conflict of interest: None
ABSTRACT
As the global pandemic of COVID-19 progresses, apart from clinical findings, imaging also plays an equally important role in the diagnosis and management. In imaging, much of the literature is focused on chest computed tomography (CT). However, due to infection control issues and lack of availability of CT scan in many centers, bedside chest X-ray (CXR) and lung ultrasound is also being used rampantly. In cases of high clinical suspicion of COVID-19, CXR can obviate the need for CT thorax. Additionally, in areas around the world with limited access to reliable reverse transcriptase polymerase chain reaction COVID-19 testing, radiological imaging becomes crucial for diagnosis and follow-up. This article describes the most common manifestations and patterns of lung abnormalities on CXR, CT thorax, and lung ultrasound in a suspected case of COVID-19 pneumonia. Early evidence suggests that initial CXR will show abnormality in most patients. The corresponding CT scan can pick up findings that may be overlooked in CXR. The progression of the disease is assessed by follow-up CT scans/X-rays. Progression and regression of disease process can be monitored by a combination of imaging modalities that facilitate clinicians to tailor management protocols.
Keywords: Consolidation, COVID-19, Ground-glass opacities, Pneumonia..
COVID-19 is caused by a virus known as 2019 novel coronavirus/SARS-CoV2 (Severe acute respiratory syndrome coronavirus 2). The disease varies in severity from asymptomatic/mild flu-like illness to severe pneumonia that can be sometimes fatal. This highly infectious virus can cause pneumonia with increased morbidity in patients with previous medical comorbidities and chronic illness. Fever, dry cough, and dyspnea are the most common clinical features of this disease.1 The real-time reverse transcriptase polymerase chain (RT-PCR) reaction test is considered to be the gold standard test for detecting COVID-19 infection, but it does not have 100% sensitivity nor specificity.2
ROLE OF IMAGING IN COVID-19
Fleischner society has given the following guidelines for imaging in COVID-19.3
- Imaging is not indicated in patients with suspected COVID-19 and mild clinical features unless they are at risk for disease progression.
- Imaging is indicated in a patient with COVID-19 and worsening respiratory status.
- In a resource-constrained environment, imaging is indicated for medical triage of patients with suspected COVID-19 who present with moderate–severe clinical features and a high pretest probability of the disease.
IMAGING MODALITIES
X-ray, ultrasound, and computed tomography (CT) chest are the common imaging modalities used in the diagnosis and follow-up of COVID-19 pneumonia. The salient features are described below.
Chest X-ray
Chest X-ray can be insensitive in the early course of the disease and can be primarily used in follow-up of cases and to look for progression of disease and its complications such as acute respiratory distress syndrome.4 Chest X-ray has lower sensitivity and specificity when compared to RT-PCR/CT chest5
One of the most unique and somewhat specific features of COVID-19 pneumonia is the high frequency of peripheral lung involvement, often mirroring other inflammatory processes such as organizing pneumonia. Such peripheral lung opacities also tend to be multifocal, either patchy or confluent, and can be readily identified on CXR.5
To conclude the CXR findings:6
- Normal CXR is noted in many cases even if CT has ground-glass opacities.
- Ground-glass opacities with or without consolidations involving predominant lower zones (Fig. 1)
- Bilateral lung involvement is seen in majority of the cases (Fig. 2).
- High frequency of peripheral lung involvement (Fig. 3).
- No pleural effusion/abscess/lung nodules.
- Lower zone OR lower and upper zone involvement is noted in most cases.
Terms such as irregular, patchy, hazy, reticular, and widespread ground-glass opacities should be used while describing features seen on chest X-ray. Furthermore, it is noted that chest X-ray abnormalities are also seen in patients whose initial RT-PCR was negative. Although further studies are required, in a suspected case of COVID-19, a positive CXR may eliminate the need for a CT.
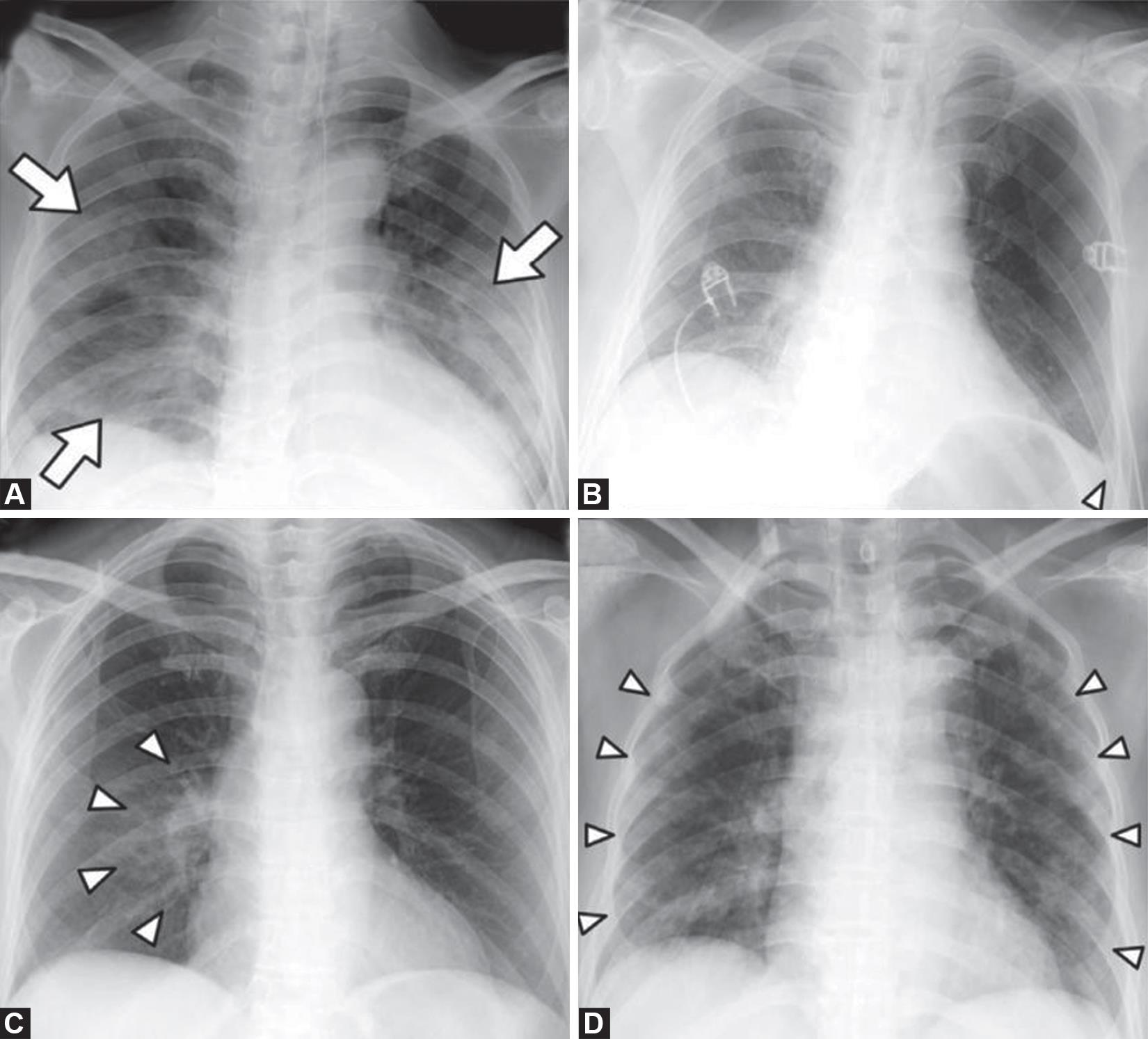
Figs 1A to D: Chest X-ray findings in COVID-19: (A) Patchy consolidations; (B) Pleural effusion; (C) Perihilar distribution; (D) Peripheral distribution. Courtesy5

Fig. 2: Chest X-ray PA view shows bilateral lung opacities that appear more evident in the peripheral areas. Courtesy: Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, Fachinetti C, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open 2020;7:100231
As the pandemic progresses, the medical community will frequently rely on portable CXR due to its widespread availability and reduced infection control issues that currently limit CT utilization.7
Ultrasound of the Lung
Lung ultrasound can predict early interstitial pneumonia. The following findings can be found in lung ultrasound in COVID pneumonia.8
- Thickening of the pleural line with pleural line irregularity (Fig. 4)
- B lines in a variety of patterns including focal, multifocal, and confluent
- Consolidations in a variety of patterns, including multifocal small, non-trans lobar, and trans lobar with occasional mobile air bronchograms
- Appearance of A lines during recovery phase
- Mixed pattern with A- and B lines can also be seen (Fig. 5)
- Pleural effusions are uncommon, and
- Subpleural consolidation with thickened pleural line.
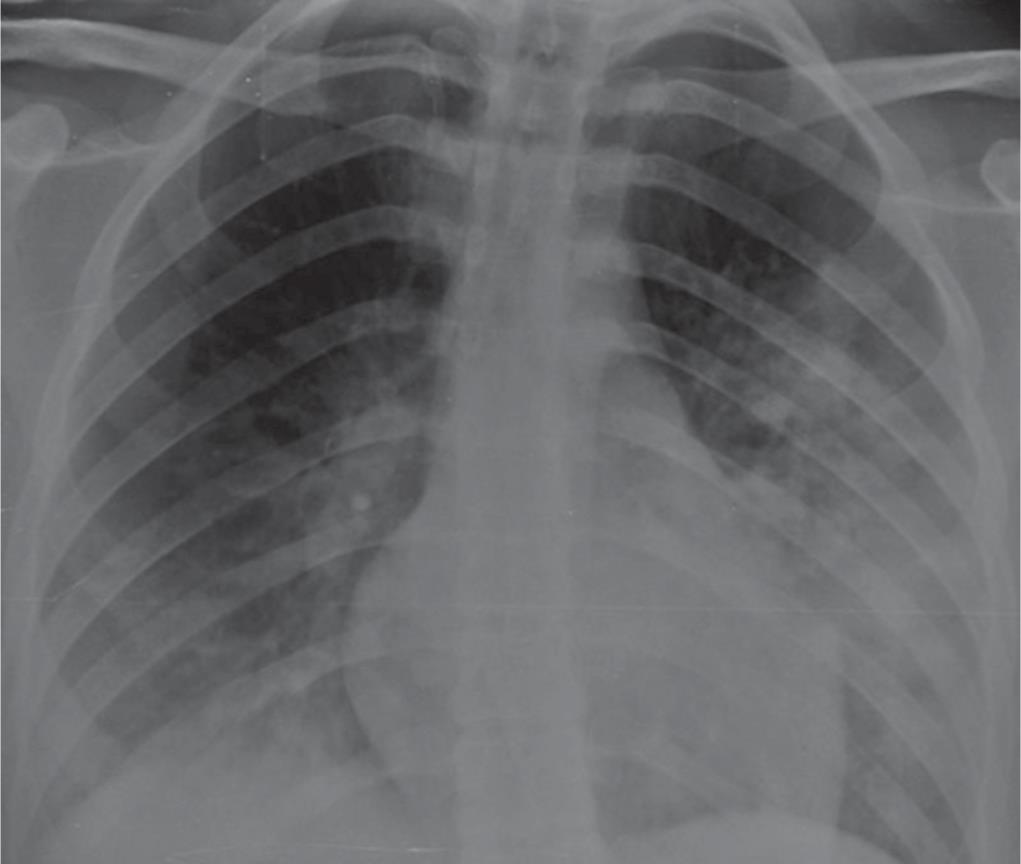
Fig. 3: Eighteen-year-old female with a fever and cough for 7 days nonresponsive to antibiotic therapy, without other known comorbidities neither relatives with similar symptoms. Chest X-ray shows bilateral opacities mainly peripheral and more evident in the left lung. Courtesy: Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, Fachinetti C, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open 2020;7:100231
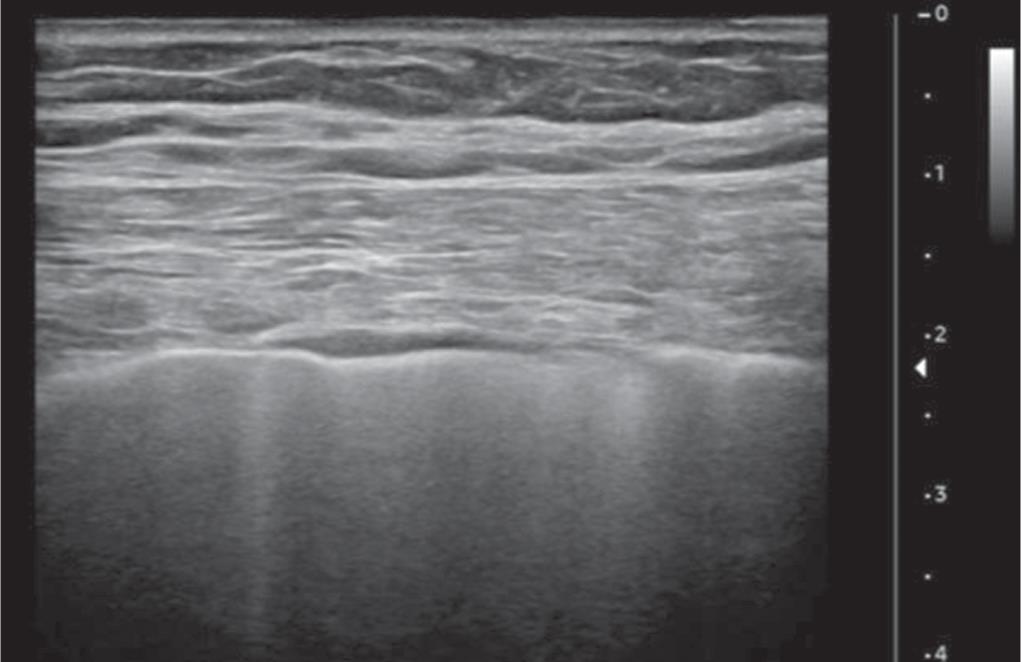
Fig. 4: Ultrasound thoracic examination using a linear transducer of a patient with COVID-19 shows the irregular appearance of the pleural line with multifocal B-line. Courtesy: Lomoro P, Verde F, Zerboni F, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open 2020;7:100231

Fig. 5: Ultrasound evaluation of lung parenchyma using the convex transducer in a patient with COVID-19 shows the simultaneous coexistence of multiple lung B lines and A lines. Courtesy: Lomoro P, Verde F, Zerboni F, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open 2020;7:100231
Computed Tomography of the Chest
Computed tomography of the chest can be normal in the initial first two days of the infection.9 In the initial phases of the disease, the predominant CT findings are bilateral peripheral, subpleural basal dominant ground-glass opacities. Later on, about 9–13 days after the onset of infection, the disease can progress to crazy paving pattern/consolidation. About 1 month after the onset of the disease, clearing of the opacities can be seen. Findings of CT of tree in bud pattern, pleural effusion, and mediastinal lymphadenopathy should arise the suspicion of superadded bacterial infection.9 Compared to non-COVID-19 pneumonia, COVID-19 pneumonia has a more peripheral distribution of ground-glass opacity (GGO) or consolidation or both, fine reticular opacity, vascular thickening, and reverse halo sign but less likely to have a central and peripheral distribution, air bronchogram, pleural thickening, and pleural effusion.10,11
Ground-glass opacities and consolidation were predominant in the early stages of the disease, whereas in advanced-phase disease showed increased frequency of GGO plus a reticular pattern, vacuolar sign, fibrotic streaks, air bronchogram, bronchus distortion, a subpleural line, a subpleural transparent line, and pleural effusion, but GGO was significantly decreased.12 The CT findings of COVID pneumonia shows that both lung parenchyma and interstitium were affected.
Computed tomography can also play a role in detecting COVID infections in strong clinically suspicious cases but with negative RT-PCR.
HRCT thorax findings which favors diagnosis of COVID-19:11,13–16 (Figs 6 and 7)
- Bilateral and peripheral distribution.
- Lesion size greater than 10 cm.
- Involvement of 5 lobes.
- Presence of hilar and mediastinal lymph node enlargement.
- No pleural effusion.
- Bilateral and diffuse involvement.
- Mixed pattern of attenuation.
Common CT signs of the COVID-19:17
- Lobular distribution
- Subpleural distribution.
- Diffuse distribution.
- Parallel pleura sign: lesions show subpleural distribution with maximum diameter of the lesion being parallel to the pleura.
- Paving stone sign: lesion mainly involves the interlobular septum.
- Air bronchogram and bronchiectasis: air bronchogram can be seen without bronchial obstruction, but it is nonspecific. Bronchiectasis can be seen in late repair stages in periphery due to traction.
- Vascular sign: thickening of vessels and telangiectasia can be seen due to inflammation.
- Halo sign and reversed halo sign.

Figs 6A to D: Unenhanced computed tomography (CT) images from patients with COVID-19 pneumonia. (A and B) A 59-year-old woman. (A) CT image of the mediastinum showing a mediastinal enlarged lymph node; (B) CT image of lung parenchyma showing multi-focal crazy-paving pattern and consolidation; (C and D) A 70-year- old woman; (C) CT image of the mediastinum showing a mediastinal and right hilar enlarged lymph node; (D) CT image of the lung parenchyma showing multifocal ground-glass opacity (GGO), crazy-paving pattern, and consolidation. Courtesy: Li X, Fang X, Bian Y, Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol 2020 May 12
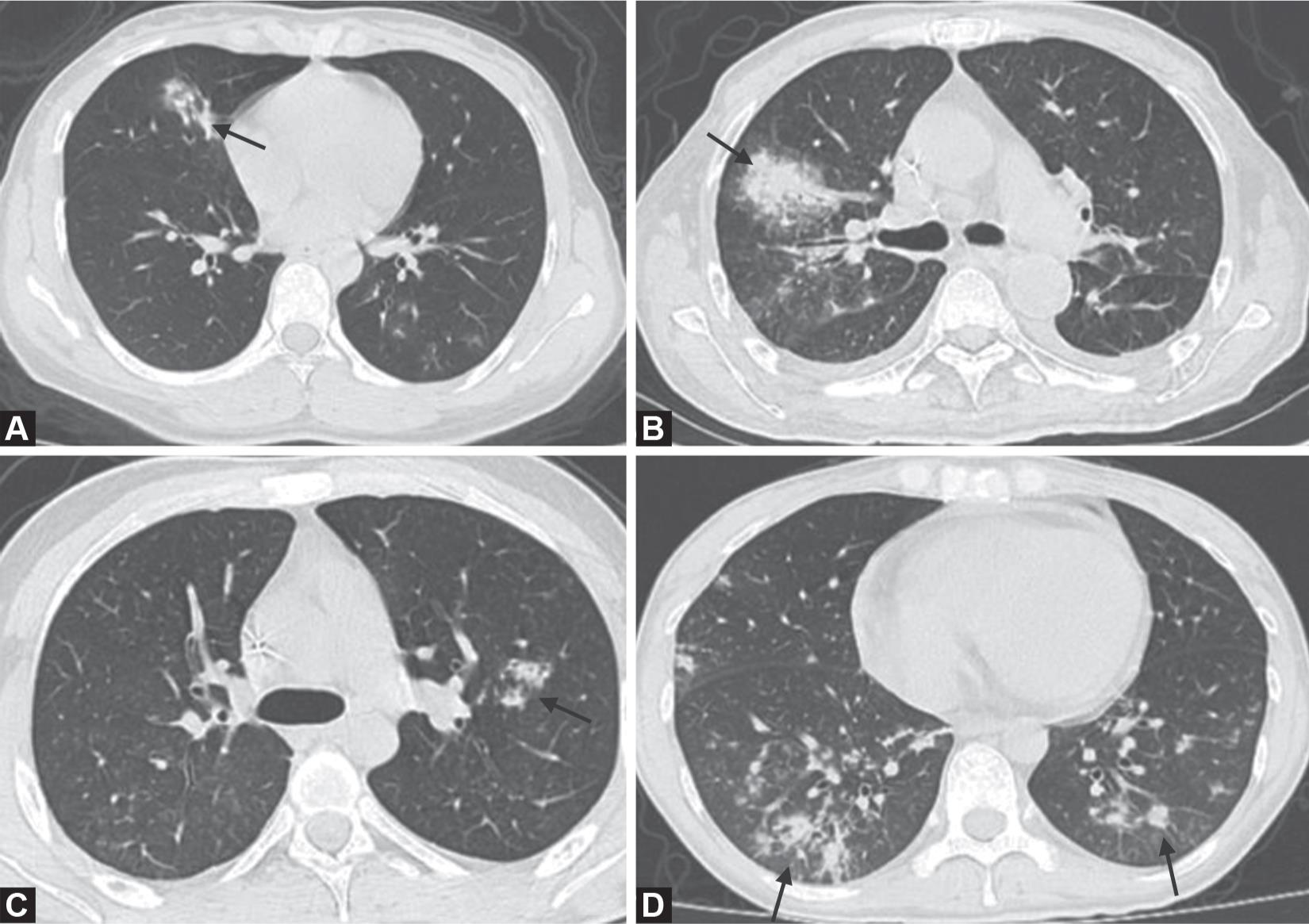
Figs 7A to D: Unenhanced computed tomography (CT) images of lung parenchyma from patients with other types of viral pneumonia. (A) CT image of a 23-year-old woman with influenza infection showing consolidation in the right middle lobe and ground-glass opacity (GGO) in the left inferior lobar; (B) CT image of a 64-year-old man with Epstein-Barr virus infection showing a mixed pattern of GGO and consolidation in the right middle lobe; (C) CT image of a 20-year-old man with adenovirus infection showing consolidation in the left inferior lobe; (D) CT image of a 24-year-old man with cytomegalovirus infection showing multi-focal GGO and consolidation. Courtesy: Li X, Fang X, Bian Y, Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol 2020 May 12

Figs 8A to D: Computed tomography (CT) images of a 25-year-old man from disease onset (day 2) to exacerbation (day 15). (A and B) The CT images at disease onset. (C and D) The CT images after exacerbation. These images indicate that the density of some patches of consolidation decreased, but the range increased significantly after exacerbation. CT scores from disease onset to exacerbation were 4 and 16, respectively. Courtesy: Wu J, Pan J, Teng D, Xu X, Feng J, Chen Y-C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia. Eur Radiol [Internet] 2020 May 4
CT Findings seen after exacerbation of covid-19 when compared with previous images18 (Fig. 8):
- Increase in GGO with consolidation
- Bilateral distribution
- Multifocal lesions
- Increase in patchy shadowing
- Air bronchogram sign
- Increase in number of involved lobes.
CONCLUSION
Majority of the COVID-19 suspected cases present with fever, cough, shortness of breath, and sore throat and RT-PCR is a major diagnostic tool to confirm these cases. Due to increasing number of false-negative cases, a combination of RT-PCR, clinical features, and imaging modalities such as chest radiograph, ultrasound chest, and CT thorax could help clinicians diagnose cases and treat accordingly. Furthermore, in cases of high clinical suspicion of COVID-19, a positive CXR may obviate the need for CT.2 Additionally, CXR utilization for early disease detection may play a vital role in areas with limited access to reliable RT-PCR COVID testing. If there is high clinical suspicion of COVID-19 with negative RT-PCR and inconclusive chest radiograph, clinicians prefer ordering for a CT chest. However, chest CT has limited sensitivity and negative-predictive value early after symptom onset.19 Bedside ultrasonography of the chest for early diagnosis is becoming increasingly popular in the emergency departments of most hospitals. Lung ultrasound allows clinicians and radiologists to identify early signs of interstitial pneumonia.6,8
Hence, the combination of the above-described imaging modalities along with clinical features in suspected cases have a high sensitivity and specificity in detection of pneumonia in COVID-19 cases.
REFERENCES
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. DOI: 10.1016/S0140-6736(20)30183-5.
2. Tahamtan A, Ardebili A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev Mol Diagn 2020;20(5):453–454. DOI: 10.1080/14737159.2020.1757437.
3. Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Radiology 2020;296(1):172–180. DOI: 10.1148/radiol.2020201365.
4. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol 2020;215(1):87–93. DOI: 10.2214/AJR.20.23034.
5. Wong HYF, Lam HYS, Fong AH-T, Leung ST, Chin TW-Y, Lo CSY, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology 2019. 201160. DOI: 10.1148/radiol.2020201160.
6. Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, Fachinetti C, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open 2020;7: 100231. DOI: 10.1016/j.ejro.2020.100231.
7. Jacobi A, Chung M, Bernheim A, Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): a pictorial review. Clin Imaging 2020;64:35–42. DOI: 10.1016/j.clinimag.2020.04.001.
8. Peng Q-Y, Wang X-T, Zhang L-N. Chinese critical care ultrasound study group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med 2020;46(5):849–850. DOI: 10.1007/s00134-020-05996-6.
9. Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. Radiology 2020. 200527. DOI: 10.1148/radiol.2020200527.
10. Li X, Fang X, Bian Y, Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol 2020. 1–9.
11. Franquet T. Imaging of pulmonary viral pneumonia. Radiology 2011;260(1):18–39. DOI: 10.1148/radiol.11092149.
12. Zhou S, Wang Y, Zhu T, Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, china. AJR Am J Roentgenol 2020;214(6):1287–1294. DOI: 10.2214/AJR.20.22975.
13. Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020;47(5):1275–1280. DOI: 10.1007/s00259-020-04735-9.
14. Shi H, Han X, Zheng C. Evolution of CT manifestations in a patient Recovered from 2019 NovelCoronavirus (2019-nCoV) pneumonia in Wuhan, china. Radiology 2020;295(1):20–20. DOI: 10.1148/radiol.2020200269.
15. Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020;295(1):18–18. DOI: 10.1148/radiol.2020200236.
16. Duan Y, Qin J. Pre- and posttreatment chest CT findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 2020;295(1):21. DOI: 10.1148/radiol.2020200323.
17. Wu J, Pan J, Teng D, Xu X, Feng J, Chen Y-C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia. Eur Radiol 2020. 1–8.
18. Liu J, Chen T, Yang H, Cai Y, Yu Q, Chen J, et al. Clinical and radiological changes of hospitalised patients with COVID-19 pneumonia from disease onset to acute exacerbation: a multicentre paired cohort study. European Radiology 2020. 1–7.
19. Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 2020. 200432. DOI: 10.1148/radiol.2020200432.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.