|
CASE REPORT |
https://doi.org/10.5005/jp-journals-10082-03151
|
A Case of COVID-19 Coagulopathy Masquerading as Acute Abdomen
1–6Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Affiliated to Sri Balaji Vidyapeeth Deemed University, Kanchipuram, Tamil Nadu, India
Corresponding Author: Sumukh Mithunkul, Department of Radiodiagnosis, Shri Sathya Sai Medical College and Research Institute, Affiliated to Sri Balaji Vidyapeeth Deemed University, Kanchipuram, Tamil Nadu, India, Phone: +91 8317356877, e-mail: sumukhmithunkul1994@gmail.com
How to cite this article: Mithunkul S, Subramaniyan V, Bala A, Shankar S, Paul J, Balaganesan H. A Case of COVID-19 Coagulopathy Masquerading as Acute Abdomen. J Basic Clin Appl Health Sci 2022;5(2):55–57.
Source of support: Nil
Conflict of interest: None
ABSTRACT
SARS-CoV-2 infection can express itself in a variety of ways, including gastrointestinal symptoms such as nausea, diarrhea, vomiting, and minor abdominal pain. Rare manifestations of SARS-CoV-2 infection have become more well-known over time. These uncommon and infrequent manifestations may make it harder to make a quick diagnosis, as well as lead to unnecessary investigations, longer hospital admissions, negative outcomes, and a greater burden on health care resources. We submitted a case to our hospital with a picture that resembled an acute abdomen, demanding surgical diagnosis and assessment. The case was found to be SARS-CoV-2 positive and did not require surgery. The importance of abdominal symptoms in the context of coronavirus disease-2019 (COVID-19) has been discussed for better evaluation of COVID-related conditions.
Keywords: Coagulopathy, COVID-19, Omental infarction.
BACKGROUND
The World Health Organization (WHO) proclaimed COVID-19 an official pandemic on March 11, 2020, after infection with the severe acute respiratory illness coronavirus.1
Coronavirus disease-2019 (COVID-19) is well-known for causing respiratory pathology, but it can also cause a variety of extrapulmonary symptoms.2 Acute coronary syndromes, acute renal injury, gastrointestinal symptoms, hepatic injury, hyperglycemia and ketosis, neurologic disorders, ocular symptoms, and dermatologic problems are among them.3
CASE DESCRIPTION
A 65-year-old male patient had complaints of right upper quadrant (RUQ) pain for the past 10 days and was RTPCR proven for COVID-19 infection.
On abdominal examination, tenderness was noted in RUQ with no abdominal rigidity or guarding. Another routine laboratory work up was unremarkable, except for mild elevation of C-reactive protein.
The patient was subjected to a contrast enhanced computed tomography (CECT) study and imaging of a well-defined non-enhancing, heterodense soft-tissue attenuation mass-like lesion measuring ~5.8 × 3.1 × 3.1 cm (CC × TR × AP) showing hypodense fat halo around it was noted in the subhepatic region anteromedial to the ascending colon with adjacent fat stranding (Fig. 1).
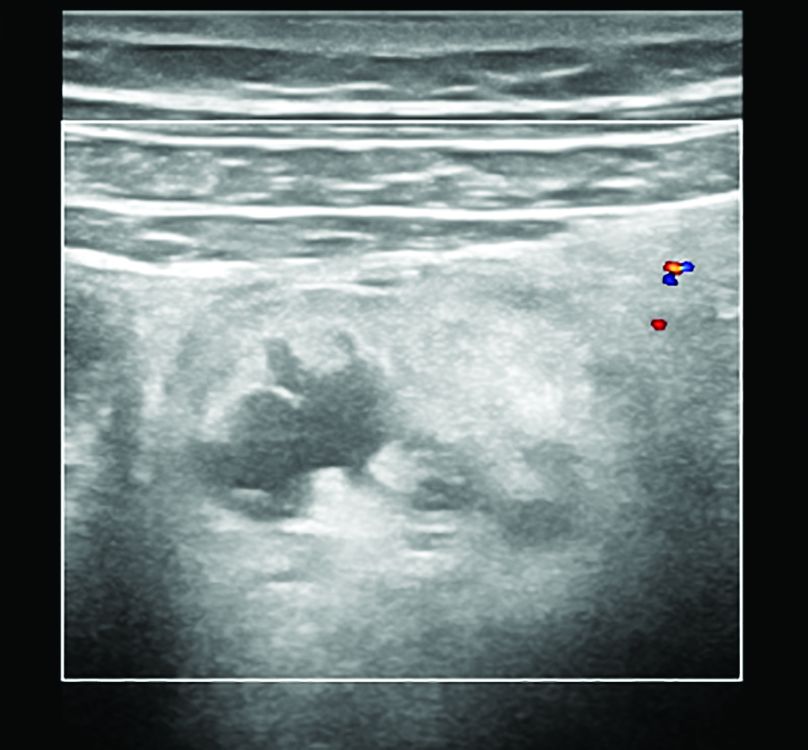
Fig. 1: Greyscale USG image showing well defined heteroechoic area with no evidence of vascularity on Doppler
Superiorly the lesion was related to the hepatic flexure of the colon and the posterior lesion was related to the ascending colon with relatively preserved fat planes. Medially lesion was related to the small bowel loops with few areas of effaced fat planes. Laterally the lesion was related to the right lateral abdominal wall musculature with relatively preserved fat planes (Figs 2 and 3)

Figs 2A and B: (A) Noncontrast-enhanced computed tomography (NECT) abdomen axial section in the soft-tissue window showing heterodense soft-tissue attenuation lesion showing hypodense fat halo in the subhepatic region anteromedial to the ascending colon with adjacent fat stranding; (B) NECT abdomen coronal reformatted image in soft tissue window showing heterodense soft-tissue attenuation lesion showing hypodense fat halo around it in the subhepatic region

Figs 3A and B: (A) CECT abdomen (arterial phase) axial section in soft tissue window showing no significant contrast enhancement of the lesion. Adjacent bowel loops show no significant abnormality; (B) CECT abdomen coronal section (portal phase) in the soft-tissue window shows no significant contrast enhancement. Adjacent bowel loops show no significant abnormality
Mildly hyperdense serpiginous structure of narrow caliber was noted coursing towards the above-mentioned lesion anteriorly suggestive of a thrombosed vessel. Small and large bowel loops adjacent to the above-mentioned lesions showed normal mural enhancement without any significant abnormality.
On ultrasound examination, the lesion appeared heteroechoic with a peripheral fat halo and adjacent inflammatory changes. No evidence of vascularity was noted within the lesion on Doppler (Fig. 1).
DISCUSSION
The coronavirus has been discovered to have an affinity for extrapulmonary angiotensin-converting enzyme 2 (ACE2) receptors, resulting in extensive involvement of numerous physiological systems due to endothelial damage and thromboinflammation, among other things.
Coronavirus disease-2019 (COVID-19) can cause gastritis, enteritis, colitis, mesenteric/omental infarction, and abdominal CECT can reveal bowel mural thickness, submucosal edema, and mucosal hyperenhancement, among other things. In the case of arterial macro thrombosis or venous blockage, severe intestine symptoms such as colon ischemia/perforation can also develop.
In our case, acute RUQ pain was caused by the creation of a microthrombus, which resulted in ischemia and omental infarction. The greater omentum is a large peritoneal fold that predominantly contain adipose tissue and blood vessels, and it connects to the stomach’s visceral peritoneal layers and the transverse colon’s visceral peritoneal layers. Because the lateral border of the omentum is freely movable and has a weaker blood supply, an omental infarct occurs largely on the right side of the abdomen, rendering it more prone to infarction and necrosis.4
Finally, COVID-19 may manifest as acute abdominal pain. In the midst of the current pandemic, clinicians should be aware of this symptom and have a low diagnostic threshold. Failure to recognize such a diagnosis could result in incorrect triage, resulting in increased morbidity and mortality.5
Final Diagnosis
Intraperitoneal focal fat infarction/omental infarction.
CLINICAL SIGNIFICANCE
In COVID-19 patients, imaging frequently reveals coagulopathy symptoms. Multisite involvement is seen in more than one-fifth of patients with such symptoms. Clinical factors aren’t very good at predicting which patients will have positive imaging results, implying that imaging has a role to play in diagnosing COVID-19-related coagulopathy. In the absence of imaging contraindications, lung CTA, extremities Doppler ultrasonography, contrast-enhanced abdomen CT, contrast-enhanced brain MRI, and MRA may all be suitable in COVID-19 patients with suspected systemic coagulopathy.6
ORCID
Sumukh Mithunkul https://orcid.org/0000-0001-6966-2182
Subramaniyan V https://orcid.org/0000-0003-0182-8216
Harshavardhan Balaganesan https://orcid.org/0000-0001-7738-5154
REFERENCES
1. Revzin MV, Raza S, Srivastava NC, Warshawsky R, D’Agostino C, Malhotra A, et al. Multisystem imaging manifestations of COVID-19, part 2: from cardiac complications to pediatric manifestations. Radiographics 2020;40(7):1866–1892. DOI: 10.1148/rg.2020200195.
2. Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 2020;395(10228):e52. DOI: 10.1016/S0140-6736(20)30558-4.
3. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS,et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020;26(7):1017–1032. DOI: 10.1038/s41591-020-0968-3.
4. Kamaya A, Federle MP, Desser TS. Imaging manifestations of abdominal fat necrosis and its mimics. Radiographics 2011;31(7):2021–2034. DOI: 10.1148/rg.317115046.
5. Ahmed AO, Badawi M, Ahmed K, Mohamed MFH. Case report: COVID-19 masquerading as an acute surgical abdomen. Am J Trop Med Hyg 2020;103(2):841. DOI: 10.4269/ajtmh.20-0559.
6. O’Shea A, Parakh A, Hedgire S, Lee SI. Multisystem assessment of the imaging manifestations of coagulopathy in hospitalized patients with coronavirus disease (COVID-19). Am J Roentgenol 2021;216(4):1088–1098. DOI: 10.2214/AJR.20.24132.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.